Cleanroom News, FDA
COVID-19, Stress, and the Fall of Zantac
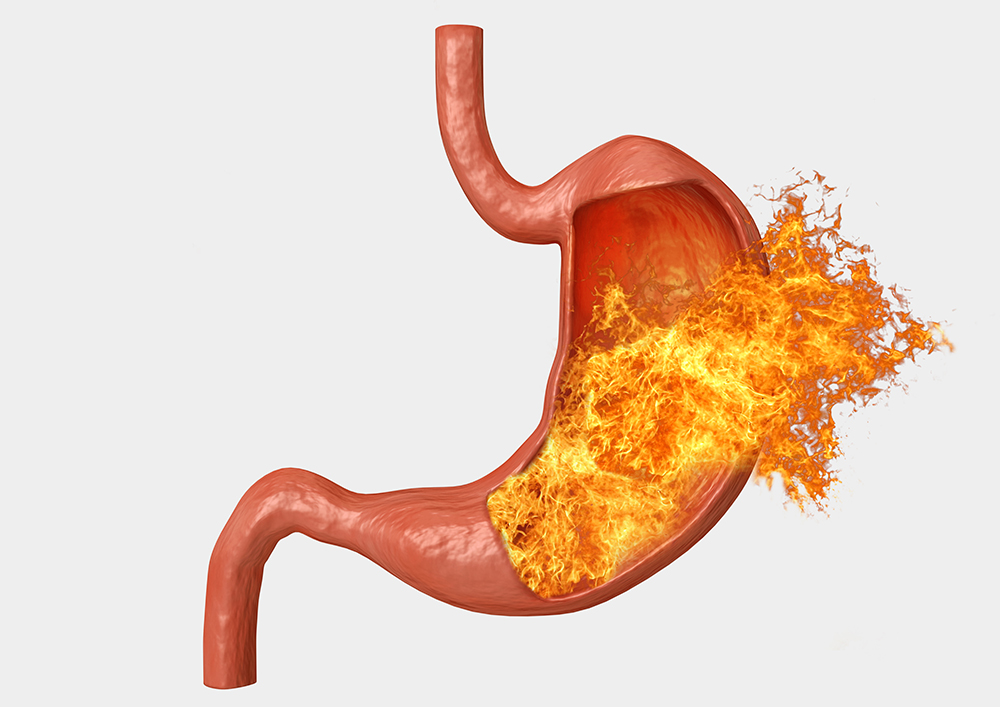
Fire in the Belly
With the global situation as it is right now, flicking on the TV, tuning into the radio, or scrolling through a social media feed is enough to send most of us into a tailspin. Between being quarantined and socially distant, home schooling kids in addition to full-time work, fears about job security or the latest run on grocery supplies, and wondering if the stress will get us before the virus does…well, suffice to say that anxiety can be a bit overwhelming. And stress rarely travels alone, preferring instead the company of its associates – headaches, loss of sleep and GI dysfunction. So it’s not surprising that many of us have been reaching for heartburn medications recently. Zantac, for example, is a popular remedy for that fire in the stomach that radiates up through your chest and into your neck. And in general it works – until it doesn’t. At a time of global anxiety and fear, shortages of medications for elevated blood pressure or gastro-intestinal pain is pretty much the last thing we need. But pharmaceutical recalls have happened and this is what you need to know…
Approved for use by the Food and Drug Administration (FDA) in 1983, Zantac was initially utilized for the treatment of Zollinger-Ellison syndrome in which tumors known as gastrinomas cause the stomach to over-produce acid, leading to abdominal pain, bleeding, peptic ulcers, and heartburn. Within just five short years, Zantac became the first drug ever to generate more than $1 billion in annual sales and, when manufacturer GlaxoSmithKine’s patent expired in 1997, multiple generic formulations were launched to exploit the market. However, according to an article published by Reuters, there was a problem.(1) In 2018, Valsartan, a treatment for elevated blood pressure, was suddenly withdrawn due to the presence of a carcinogen, N-nitrosodimethylamine (NDMA). What does this have to do with heartburn? The same impurity was subsequently detected in multiple drugs in the same class as Valsartan – Angiotensin II Receptor Blockers (ARBs) – including ranitidine, popularly branded as Zantac.
Not to be confused with MDMA (‘Ecstacy’), NDMA is an organic compound that is a member of the N-nitrosamine class.
It is recognized as a hepatoxin that has been shown in animal test subjects to cause tumors and fibrosis of the liver. It occurs commonly in groundwater proximal to rocket launch sites and in drinking water that is treated with chlorination, and contamination is especially problematic insofar as there is no general consensus regarding a maximal contaminant level, or MCL. In California, the MCL is set at 10 nanograms/liter whereas the Environmental Protection Agency (EPA) has not yet committed to an absolute level, recommending only that the maximal admissible concentration be 7 ng/L. Defined in Section 302 of the U.S. Emergency Planning and Community Right-to-Know Act (42 U.S.C. 11002) as an ‘extremely hazardous’ substance, facilities using, storing, or producing NDMA are mandated to report it with a view to emergency response preparedness. In short, this is not exactly a palatable substance.
However, somehow, it found its way into a best-selling remedy for heartburn.
How this occurred remains uncertain. Some researchers support the idea that it was introduced during the manufacturing process, especially given that much of the active pharmaceutical ingredient (API) is manufactured overseas in facilities that may not have the same level of oversight as domestic manufacturers. Saraca Laboratories Ltd., based in Hyderabad, India, is a leading manufacturer of Ranitidine HCl, producing 3600 tons per annum according to the company’s website. And, according to the company’s own marketing materials, it seems they have impressive facilities: ‘[At Saraca] production buildings have finished product areas for APIs with clean air, purified water systems that operate under full cGMP as per ICH guidelines. It has cooling services, brine, cool water, heating with thermal oil or steam, 100% standby power, warehouses & bulk solvent storage tank farms. The facility is included with environmental friendly Vapour Absorption system for chilling applications.’ Corporate literature also states that the facilities are approved by ‘USFDA, KFDA, TGA & WHO-GMP.’(2) Other overseas manufacturers mentioned in connection with the Zantac recalls include Sandoz, a subsidiary of Switzerland-based Novartis, and Sanofi, which is headquartered in France.
And with global manufacturing and supply chains comes global distribution so when a problem in identified in one country, recalls are often replicated elsewhere. And this was certainly true in the present case. In 2019, distribution of heartburn medications containing the potentially contaminated ingredient was halted worldwide, with major domestic drugstore chains such as CVS, Rite Aid, and Walgreens taking any over the counter (OTC) medications containing ranitidine off their shelves regardless of branding. But recalling the affected products is only step #1: identifying how the ranitidine became contaminated is step #2.
At this time, the FDA remains unsure as to the source of the NDMA, however analysis has shown that it was ‘present in both the finished drug product samples and the active pharmaceutical ingredients (APIs).’(3)
Additional testing ‘simulated gastric fluid and simulated intestinal fluid [and] results illustrated that NDMA was not formed in the conditions of the stomach or the intestines.’(4) Under certain circumstances, NDMA can be produced within the body – an example of which is the digestion of some foods, including beer, fish, and cured meats. In the case of the latter, meats are cured with sodium nitrite to prevent the threat of botulism and this leads to a release of nitrous acid in the stomach. As proteins are broken down in the gut, the acid combines with dimethylamine and NDMA is formed. However, in the case of the recalled Zantac the FDA’s analysis indicates that the contamination was not a problem of physical breakdown or drug metabolism within the body but more likely present before ingestion. In an article published in FiercePharma, an online news source covering the biopharmaceutical industry, senior editor Eric Palmer writes that an independent lab in Alameda, CA, petitioned the FDA reporting that ‘preliminary data indicate that NDMA accumulates in ranitidine-containing drug products on exposure to elevated temperatures, which would be routinely reached during shipment and during storage. More importantly, these conditions occur post-lot release by the manufacturer. Hence, while NDMA levels in ranitidine may be acceptable at the source, they may not be so when the drug is purchased and subsequently at the time of consumption by the consumer.’(5) To corroborate these findings, an article published by CNN states that initial tests ‘didn’t observe unacceptable levels of NDMA in many of the samples’ but the FDA did determine that levels of the carcinogen can actually increase.(6) Per the agency’s website: ‘FDA laboratory tests show that temperature and time generally raise the level of NDMA in some ranitidine products above the acceptable daily intake limit of 96 nanograms per day.’(7)
So what does this mean in terms of the risk level associated with the ingestion of NDMA-tainted ranitidine? The FDA states the following: ‘FDA does not expect nitrosamines to cause harm when ingested at low levels. Nitrosamine impurities may increase the risk of cancer if people are exposed to them at above acceptable levels and over long periods of time, but a person taking a drug that contains nitrosamines at, or below, the acceptable daily intake limits every day for 70 years is not expected to have an increased risk of cancer.’(8)
This may be so but it seems like cold comfort, particularly to those who are reliant upon the medication but anxious about the implications of the tainted products.
So what actions does the FDA recommend in the face of these recalls?
According to its website, while the agency is advising consumers who take OTC ranitidine products to discontinue their use with immediate effect, those ‘taking prescription ranitidine should speak with their health care professional about other treatment options before stopping the medicine.’(9) Usually in these cases, manufacturers suggest returning products to designated ‘drug take-back locations’ but, in the face of COVID-19 social distancing and quarantine, CNN reports that users should follow the disposal guidelines included with the product.
However, the N-nitrosodimethylamine saga doesn’t end there. In February of this year, the FDA revisited the topic of NDMA contamination, this time in connection with metformin, a drug used very widely in the treatment of type 2 diabetes. With an estimated 30 million diabetics in the US (of whom 90% to 95% use metformin), the scale of users potentially affected is significant. Where alternatives to Zantac do exist – viz famotidine (Pepcid), cimetidine (Tagamet), esomeprazole (Nexium), lansoprazole (Prevacid), and omeprazole (Prilosec) – metformin is a whole different problem. As the only biguanide currently licensed for use in diabetes management, metformin is prescribed under the brand names Glucophage, Glucophage XR, Glumetza, Riomet, and Fortamet to both reduce the amount of glucose released by the liver and to increase its uptake into cells. The drug, in essence, prevents the conversion of fats and amino acids to glucose, at the same time as activating the enzyme AMPK which elevates the body’s sensitivity to insulin. Clearly, absent therapeutic intervention through dietary and lifestyle changes, metformin is the go-to treatment for the management of diabetes.
However, according to Medscape Medical News, an online repository of clinical reference and medical news, three versions of metformin were recently recalled in Singapore, prompting the European Medicines Agency to request that manufacturers test for the presence of NDMA. According to information from the FDA, the agency has tested ten metformin products from seven manufacturers and has concluded that only two – Rx Metformin 1000mg ER and Rx Metformin 500mg ER – have detectable levels of NDNA. The products are manufactured by Actavis, whose parent organization Teva Pharmaceuticals is headquartered in Parsippany-Troy Hills, NJ. For a more detailed analysis, see the FDA’s breakdown here.
While accepting that processes are inherently imperfect and can always be improved, it is interesting that it would fall to an independent laboratory – Emery Pharma – to require action by the FDA through the use of a Citizen Petition to the agency. However, precisely this was deemed necessary given that the impurity had not been caught sooner. In its own defense, the FDA notes: ‘As testing methods have become more sophisticated and sensitive, FDA and industry can identify and mitigate previously-unknown risks to patients.’(10) Or, in other words, now that we know better, we can do better. It’s concerning, however, that once again it takes a small third-party like Emery Pharma to sound the alarm and force the agency’s hand.
If the current situation is giving you heartburn, how are you managing without Zantac? Are you concerned by the levels of NDMA reported in the drug? Or do you feel that the FDA has the situation under control? Let us know your thoughts!
References:
- https://www.reuters.com/article/us-health-fda-heartburn-timeline/timeline-popular-heartburn-medicine-zantac-pulled-off-store-shelves-idUSKBN1X014E
- https://www.saraca.com/facilities.htm
- https://www.fda.gov/drugs/drug-safety-and-availability/questions-and-answers-ndma-impurities-ranitidine-commonly-known-zantac
- ibid
- https://www.fiercepharma.com/manufacturing/lab-finds-ndma-zantac-can-develop-during-storage-bloomberg
- https://www.cnn.com/2020/04/01/health/zantac-fda-remove-from-market-bn/index.html
- https://www.fda.gov/drugs/drug-safety-and-availability/questions-and-answers-ndma-impurities-ranitidine-commonly-known-zantac
- ibid
- ibid
- https://www.fda.gov/drugs/drug-safety-and-availability/questions-and-answers-ndma-impurities-ranitidine-commonly-known-zantac

















HAVE AN IDEA FOR CONTENT?
We are always looking for ideas and topics to write about.
Contact Us